The "Science" Behind the Headlines
Untangling the art of burying propaganda in science
It has become somewhat of a cliche in scientific studies relating to COVID-19 vaccination, to remind readers of the significant “benefits outweighing the risks” and the “millions of lives saved by COVID-19 vaccination”.
These propaganda inserts in scientific studies are likely the result of a range of conscious and subconscious biases which we will explore in this article, focusing specifically on an example from a recent preprint from Australia.
The preprint in question provides an exemplar of doublethink, where science is twisted to fit a narrative that COVID-19 vaccination is both safe and effective as though 2 + 2 = 5.
The preprint “Effectiveness of COVID-19 Vaccination Against COVID-19 Specific and All-Cause Mortality in Older Australians”, authored by a collection of epidemiologists, health bureaucrats and academics, commissioned by Australia’s premier vaccine propaganda institute, The National Centre for Immunisation Research and Surveillance (NCIRS); and, funded by the Australian Federal Government Department of Health and Aged Care, asserts that COVID-19 vaccination has reduced all-cause mortality in Australia, despite the record excess mortality in Australia in 2022.
The title of the preprint would seem to suggest that the authors could make a compelling case against the benefits of COVID-19 vaccination, given the extraordinary rates of excess mortality in 2022, particularly in “older Australians”.
But alas, the authors do no such thing, and instead make the following startling claims which appear so detached from reality they have to be read, repeatedly, to be believed:
“COVID-19 vaccination is highly effective in preventing COVID-19 death and also reduces all-cause mortality.” [emphasis added]
“COVID-19 vaccination was also found to be effective against all-cause mortality.”1 [emphasis added]
So just how do they arrive at such alarmingly outlandish claims?
Study exclusions
First, exclude those from the study who might negatively impact the “safe and effective” propaganda:
Those under the age of 65 “as there were relatively few deaths in those ages”2 (>13.5 million people aged under 65 during the study, 28,096 deaths in this cohort during the study period [1,356 deaths above the baseline3]);
Those who had received five or more vaccine doses (>2,400 people excluded);
Those who received only 1 dose (47,294 people excluded); and,
Those with significant missing data (> 2.5 million people excluded).4
Study design
Second, choose a study design called “survival analysis”, where you assess how long it takes the study participants to die (if at all) against how recently they took a COVID-19 vaccine (if at all) and then, having determined that interval, compare who had better outcomes (survival, death from COVID-19 or death from other causes).
But survival analysis in this context is problematic. COVID-19 has a survival rate exceeding 99% - even for aged Australians - and more than 11 million people had been infected in Australia by the end of 2022. As the majority of cases recovered naturally, the small proportion of severe cases or fatalities may not provide enough statistical power to detect meaningful differences.
Another critical challenge is the potential for wrongly attributing survival solely to COVID vaccination. When a substantial proportion of individuals recover without vaccination, it becomes challenging to disentangle the impact of vaccination from other factors contributing to survival, such as individual immunity, or the evolving nature and lethality of the virus itself.
Ignore negative vaccine effectiveness
Third, omit any discussion of the risks or adverse effects of vaccination, despite the results in the study showing negative vaccine effectiveness for specific causes of death such as cancer, cerebrovascular disease, ischaemic heart disease, dementia, respiratory disease, and even COVID-19 for some cohorts - all of which were the major contributors to excess mortality in Australia in 2022, especially for older Australians.
The study calculated “vaccine effectiveness” (VE) by measuring the overall reduction in the risk of death in the vaccinated (2 doses, 3 doses or 4 doses) group compared to the unvaccinated group. The study estimated “adjusted hazard ratios” (aHR) to calculate VE against COVID-19 mortality, all-cause mortality, and mortality by specific causes of death using the formula:
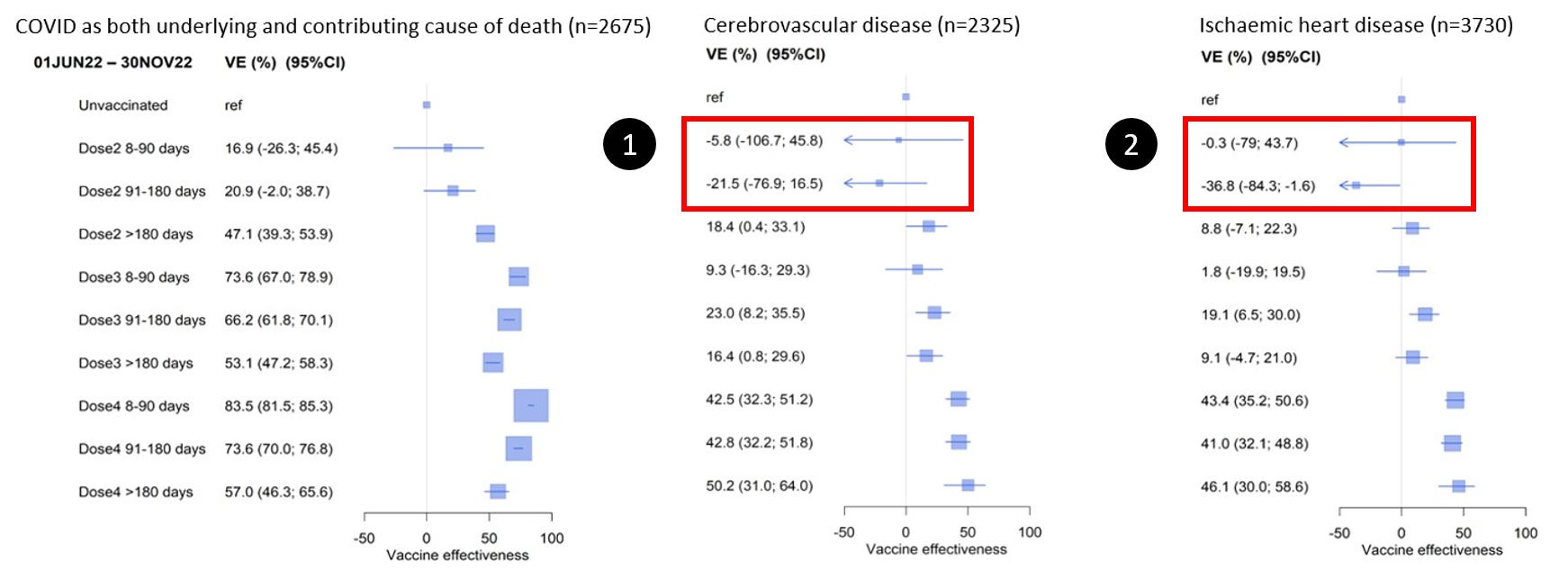
A negative VE value implies that there was a potential adverse effect associated with the vaccine for the specific group and time frame mentioned, and negative VE was observed for the specific causes of death shown below:

Cerebrovascular disease:
Dose 2 8-90 days: VE estimate of -5.8 (-106.7; 45.8): Showing an increased risk of death from cerebrovascular disease compared with those who did not receive the vaccine.
Dose 2 91-180 days: VE estimate of -21.5 (-76.9; 16.5): Similar to the previous estimate, this suggests a considerably increased risk of death from cerebrovascular disease compared with those who did not receive the vaccine.
Ischaemic heart disease:
Dose 2, 8-90 days: VE estimate of -0.3 (-79; 43.7): A slight increase in the risk of death from ischaemic heart disease within 8-90 days after receiving the second dose, but the result is not statistically significant compared with those who did not receive the vaccine.
Dose 2, 91-180 days: VE is estimated at -36.8% (-84.3% to -1.6%): Showing a considerably increased risk of death from ischaemic heart disease compared with those who did not receive the vaccine.
Dementia:
Dose 2, 8-90 days: VE estimate of -48.8 (-116.2; -2.5): Showin a significantly increased risk of death from dementia compared with those who did not receive the vaccine.
Dose 2, 91-180 days: VE is estimated at -6.4 (-40.5; 19.5): Showing an increased risk of death from dementia compared with those who did not receive the vaccine.
Respiratory disease:
Dose 2, 8-90 days: VE estimate of -3.1 (-73.2; 38.6): Showing an increased risk of death from respiratory disease compared with those who did not receive the vaccine.
Dose 2, 91-180 days: VE estimate of -12.4 (-50.4; 16.1): An increased risk of death from respiratory disease compared with those who did not receive the vaccine.
Cancer:
Dose 2, 8-90 days: VE estimate of -29.6 (-80.3; 6.8): Showing considerably increased risk of death from cancer compared with those who did not receive the vaccine.
Dose 2, 91-180 days: VE estimate of -12.6 (-36.2; 6.9): Showing an increased risk of death from cancer compared with those who did not receive the vaccine.
How do the authors treat these inconvenient results?
Ignore them.
“COVID-19 vaccines also appeared effective against other specific causes of death . . . although the magnitude of the effect size was less, and patterns of waning effectiveness were inconsistent.”5
The authors do not mention the significant evidence of negative vaccine effectiveness for the “recent” (8-90 days and 91-180 days) 2 dose cohorts in the study period June-November 2022.
Similar negative vaccine effectiveness is evident for the “recent” 2 dose cohorts relating to all-cause mortality in both study periods, and dramatic changes in VE are observed:

January-May 2022 study period:
Dose 2 > 180 days: VE estimate of -15.8 (-11.0; -20.8): Showing a moderately increased mortality risk compared with those who did not receive the vaccine.6
June-November 2022 study period:
Dose 2 8-90 days: VE estimate of -18.8 (-37.2; -2.9): Showing a moderately increased mortality risk compared with who did not receive the vaccine.
Dose 2 91-180 days: VE estimate of -11.9 (-22.0; -2.7): Showing an increased mortality risk compared with those who did not receive the vaccine.
Similarly, regarding VE:
VE for the recently (primary dose) vaccinated decreases from 72.7% to 13.9% from study period 1-2;
VE for the moderately recently (primary dose) vaccinated decreased from 65.9% to 21.8% from study period 1-2.
How do the authors explain the results showing better outcomes for the unvaccinated compared against the 2 dose cohorts shown? And how do they explain the significant reductions in VE for the cohorts who were recently vaccinated with their primary dose?
Simple: ignore them:
““VE waned with time following receipt; and waning was greater for those who only had two compared to three vaccine doses. . . We observed similar VE patterns with vaccine dose and time since receipt over the two waves for both outcomes.”7 [emphasis added]
Contrary to the above, VE did not wane “with time following receipt” for the 2 dose cohort and this evidence is not addressed anywhere in the paper.
A participant who received their primary dose between 8-180 days ago had worse protection than someone who received their primary dose more than 180 days ago with regard to both COVID-19 and all-cause mortality in both study periods.
So what might have caused this significant reduction in apparent VE?
We hypothesise these particular results demonstrate the harmful effects of COVID-19 vaccination following infection. We know that COVID-19 cases exploded in Australia in the first half of 2022, and therefore, those that received vaccination in this second study period, which was most likely after infection, would have likely had far worse mortality outcomes. The combination of recent COVID infection and vaccination might explain the significant drop in VE across the two study periods, and also, the negative vaccine effectiveness, though the data provided in this study is not complete, and this hypothesis cannot be confirmed.
It should be noted that the results in the study have wide confidence intervals, indicating uncertainty, however, this uncertainty is never acknowledged by the authors in their final recommendation for more and more COVID-19 vaccination:
“In summary, this study quantifies the effectiveness of COVID-19 vaccines against mortality in the Australian population aged 65+ years during 2022 when the SARS-CoV-2 Omicron variant dominated. We demonstrate that both the primary course and subsequent boosters provide significant protection against death from COVID-19.”8 [emphasis added]
The authors completely ignore the concerning safety signal of negative vaccine effectiveness for the 2 dose recipients compared with the unvaccinated for these specific causes of death and for all-cause mortality.
Ignore higher mortality rates in vaccinated cohorts
Fourth, the study ignores similar and significantly higher mortality rates in some cohorts, and “cherry-picks” the cohorts with perceived better outcomes. For example, consideraby worse COVID-19 mortality outcomes (compared with the unvaccinated) are dismissed for the 2 dose recipients in the second study period (June-November 2022) and for the 3 dose recipients in the first study period (January-May 2022):

January-May study period:
Dose 2 > 180 days: approximately equivalent mortality rate compared with the unvaccinated.
Dose 3 > 180 days: 23% higher COVID-19 mortality rate compared with the unvaccinated (or an 18% lower mortality risk for the unvaccinated compared with this 3 dose cohort).
June-November study period:
Dose 2, 8-90 days: 148% higher COVID-19 mortality rate compared with the unvaccinated (or a 59% lower mortality risk for the unvaccinated compared with this 2 dose cohort).
Dose 2, 91-180 days: 21% higher COVID-19 mortality rate compared with the unvaccinated (or a 17% lower mortality risk for the unvaccinated compared with this 2 dose cohort).
Diminish the importance of natural immunity
Fifth, the study does not account for past COVID-19 infections which are known to affect subsequent risk of severe disease, which would, therefore, lead to overestimates of the role of COVID-19 vaccination in reducing mortality in this “survival analysis”.9
The more than 11 million cases of COVID-19 in Australia in 2022 point to the significant role that prior infection likely played in the “survival” of the all but very old, comorbid or immunocompromised.
The authors do acknowledge, however, that prior infection may have influenced the vaccine effectiveness measurement by narrowing the “immunity gap” between unvaccinated and vaccinated participants. In other words, the VE may have decreased over time because the unvaccinated acquired some degree of protection from their infection, and, because VE is measured against the outcomes for the unvaccinated, the vaccines have the illusion of “waning effectiveness”.
The authors neglect to mention how or why those who were vaccinated and were infected with COVID-19 during this study period had worse outcomes than the unvaccinated, therefore, implicitly rejecting the purported superior protection of “hybrid immunity”.10
In other words, if the unvaccinated experienced an improvement in the many types of mortality (COVID-19, all-cause and/or by specific cause) from prior infection, then why was this protection not conferred to the 2 dose vaccinated cohort in the same manner?
The omission is made even more significant when considering the evidence of negative vaccine effectiveness discussed previously, further undermining the notion that “hybrid immunity” provides superior protection.
If natural immunity only provided gains to the unvaccinated to close the “immunity gap”, it appears that the study authors have implicitly acknowledged the evidence of negative vaccine effectiveness for the cohorts discussed previously.
Bias
Sixth, the study’s many biases, likely driven to have the findings conform to the Paradigm, limit the analysis:
The study aggregates participants into only two broad age categories (65-79 and 80+), limiting our ability to gain a nuanced understanding of the vaccination patterns and outcomes within the elderly population. Given the availability of more detailed population data in ten-year or five-year age brackets, a finer-grained age stratification could have provided valuable insights into the vaccination behaviours and risk profiles of individuals in these specific age groups.11 This finer granularity could have shed light on why certain age segments, particularly those aged over 90 for example, may have exhibited different vaccination rates, ultimately contributing to a more comprehensive analysis. Furthermore, it could have avoided the selection bias of the study in which the mortality risk associated with being unvaccinated was overestimated. For example, if older, frailer, closer-to-death individuals were less willing, or able to be vaccinated, then the mortality risk from COVID-19 would appear far worse in the unvaccinated group;
The study's exclusion of individuals who had received only one dose of the COVID-19 vaccine from the analysis of vaccine effectiveness may introduce potential censoring or classification bias. It is unclear whether these individuals are treated as censored data, thus possibly affecting the estimated mortality risk for the “unvaccinated” cohort. Additionally, this exclusion may impact the study's conclusion regarding the effectiveness of COVID-19 vaccination, particularly if adverse events related to the first vaccine dose are not considered;
The study's omission of results for vaccines received within the 0-7 day time period, citing “small numbers”12 removed an opportunity to investigate potentially important temporal associations between vaccination and mortality. Adverse events following vaccination, particularly in the immediate post-vaccination period, have been widely reported.13 Although these numbers may be relatively small compared to overall mortality, their inclusion in the analysis could have provided valuable insights into the timing and potential associations between vaccination and mortality outcomes;
The exclusion of individuals who received a fifth vaccine dose as part of an immunocompromising condition-based regimen raises questions about the potential impact on the overall estimation of vaccine effectiveness. While the authors allude to this exclusion potentially counterbalancing the healthy vaccinee effect, they do not provide a corresponding adjustment when analysing and referencing the unvaccinated population. This omission leaves room for a potential bias, as the exclusion of a potentially sicker cohort from the vaccinated group could influence the comparative results against the unvaccinated cohort.
Conclusions
The authors recommend continuing the administration of COVID-19 vaccines, including boosters, despite a significant portion of the evidence presented in the study challenging the assertion that COVID-19 vaccines are both “safe and effective”.
Despite alarming data showing negative vaccine effectiveness for specific causes of death and all-cause mortality, and higher mortality rates for selected vaccinated cohorts, the authors recommend the continuation of COVID-19 vaccination, particularly for those at highest risk.
The incongruity in the evidence presented in this study and its conclusion seemingly does not matter.
Very few people will likely read the study.
The headline provides the talking point: the science and evidence is secondary.
If ever called out on this study’s evidence, the political class will have had the time to dodge, duck, weave, manoeuvre, truth-massage and goalpost-shift their COVID-19 vaccine messaging.
They may even refer to a new, yet-to-be-posted (self) funded and favourable preprint to support their propaganda.
The cynicism is not without merit.
We find one such attempt from Australia’s Chief Medical Officer, Professor Paul Kelly, who, during Senate Estimates for the Community Affairs Legislation Committee, cited the evidence in this “recent preprint publication” in response to a question put to him about the reasons for Australia’s excess mortality:
“Clearly, it is related to the pandemic. A lot of the excess deaths that happened in 2022 were directly attributable to or related to a diagnosis of COVID, not due to the vaccine….We've got very good data now from our own research that we've funded through the National Centre for Immunisation Research and Surveillance in Sydney, with other partners across the country, which demonstrates very clearly that vaccines are incredibly protective against death. In over-65s, it leads to a 93 per cent decrease in the death rate.”14 [emphasis added]
Kelly’s response is wrong on many points:
His claim that a lot of the excess deaths were “not due to the vaccine” directly denies the evidence of negative vaccine effectiveness in the study for many leading causes of death. In the absence of complete evidence, we are not suggesting the vaccines caused the death, however, as the results show, unvaccinated participants had better all-cause mortality outcomes than the 2-dose group;
While the data shows that individuals who received two vaccine doses had worse mortality outcomes compared to those who received three doses, it raises an important question; how can the benefits of the three-dose vaccination strategy outweigh the potential risks associated with the two-dose regimen? In other words, if we are promoting the advantages of a three-dose approach, it is essential to explain how individuals can still derive these benefits if they have to run the risk of the 2 doses;
He uses results showing improvements in COVID-19 mortality and conflates these with reductions in all-cause mortality, which we determined were at best uncertain, and at worst, revealed adverse events (negative vaccine effectiveness) compared with the unvaccinated cohort;
He is guilty of selection bias when he trumpets the reduction in COVID-19 mortality whilst ignoring the alarming reduction in VE for many of the cohorts between study periods; and,
He also completely ignores the 'Unvaccinated' group had approximately 59.84% lower mortality rate compared to the 'Dose 2 8-90 days' group in the June-November 2022 study period.
This is Australia’s Chief Medical Officer trying to account for why Australia had such extraordinary excess mortality in 2022 and he gets it so badly wrong.
How, as he affirms in the exchange in the video below, can he say the “vaccines are entirely and incredibly effective”?
In light of the evidence presented in this article, what does the word “entirely” and “incredibly” with respect to the COVID-19 vaccines even mean to Professor Kelly?
At the same hearing, Dr Phillip Gould, the First Assistant Secretary of the Health Economics and Research Division had his turn parroting the talking points:
“I believe Professor Kelly might wish to make some points, but I will quickly say that the Department worked with the National Centre for Immunisation Research and Surveillance to produce a paper, which is out for preprint at the moment. That paper examines the relationship between vaccine coverage for people aged 65 or over in terms of COVID mortality but, importantly, all-cause mortality as well. That document is available for public scrutiny, and it found no link between vaccination and all-cause mortality.”15 [emphasis added]
Like Kelly, Gould overtly admits the paper’s conflict of interest and bias.
The Australian Federal Government Department of Health and Aged Care “worked with” the NCIRS to “produce a paper” to support the Government narrative.
Is it any wonder we hear the “safe and effective” tune when we know who paid the piper?
Their study found no link between vaccination and all-cause mortality: “no link”.
We know this statement is patently false.
Many of us know how to see this as propaganda, but, as long as this propaganda is allowed to continue unchallenged: it will.
Liu, Bette and Stepien, Sandrine and Dobbins, Timothy and Gidding, Heather and Henry, David and Korda, Rosemary and Mills, Lucas and Pearson, Sallie-Anne and Pratt, Nicole and Vajdic, Claire and Welsh, Jennifer and Macartney, Kristine, “Effectiveness of COVID-19 Vaccination Against Covid-19 Specific and All-Cause Mortality in Older Australians”, https://ssrn.com/abstract=4445191, accessed 28 August 2023, p. 3
Ibid.
Australian Bureau of Statistics, “Provisional Mortality Statistics Jan-Dec 2022”, https://www.abs.gov.au/statistics/health/causes-death/provisional-mortality-statistics/jan-dec-2022, accessed 2 September 2022.
It is not suggested that these individuals could/should have been included, rather, this highlights an additional limitation of this analysis because significant size of the missing data.
Liu, Bette, op. cit., p. 9
Curiously, the upper bound is displayed on the right in the confidence interval. We suspect this is in error. The VE appears to be the average of the two negative values -11 and -20.8.
Liu, Bette, op. cit. p. 7
Liu, Bette, op. cit., p. 10
Bobrovitz N, Ware H, Ma X, et al., “Protective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid Immunity against the Omicron Variant and Severe Disease: A Systematic Review and Meta-Regression”, The Lancet Infectious Diseases, 2023, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00801-5/fulltext
Australian Technical Advisory Group on Immunisation, “ATAGI Update on the COVID-19 Vaccination Program, 1 September 2023”, https://www.health.gov.au/news/atagi-update-on-the-covid-19-vaccination-program, accessed 4 September 2023.
The information is readily available and researchers would have had access to age-stratified data from the Australian Census in 2021: why wasn’t it used?
Liu, Bette, op. cit., p. 5
Australian Federal Parliament, “Community Affairs Legislation Committee - Senate Estimates 1 June 2023”, https://parlinfo.aph.gov.au/parlInfo/download/committees/estimate/26915/toc_pdf/Community%20Affairs%20Legislation%20Committee_2023_06_01.pdf;fileType=application%2Fpdf#search=%22committees/estimate/26915/0000%22, p. 16
Ibid., p. 25