Sedation, Not Salvation (Part 2)
Confirmation of the widespread use of sedatives which hastened the deaths of residents "from COVID-19" at Newmarch House aged-care facility.
In Sedation, Not Salvation (Part 1), we provided evidence that “chemical restraints” (sedatives) were used on residents in aged-care facilities in Australia, likely hastening their death “from COVID-19” and other leading causes such as dementia in 2020.
We showed how a mere positive COVID-19 test (a significantly flawed test) was all that was required for an aged-care resident to be placed on this “end-of-life” care protocol, and how “informed consent” could even be obtained after the medical intervention.
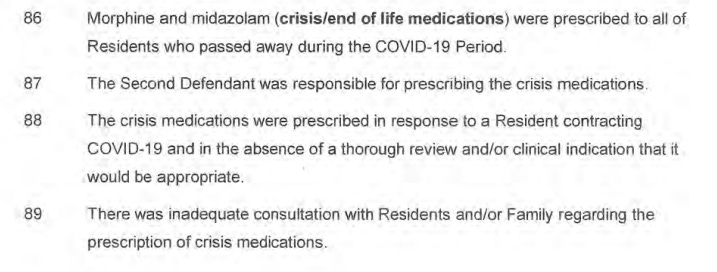
Now, the evidence from the recently concluded inquest into the deaths at one of these RACFs — Newmarch House in western Sydney, NSW — confirms the widespread use of sedatives in this particular RACF and horrifyingly, that all residents who died at this facility during this COVID-19 outbreak were prescribed Midazolam and Morphine prior to their “COVID-19 deaths”.
Despite the known risks and harms with these sedatives, particularly for those with respiratory illness or dementia, seventeen of the nineteen residents died because of their COVID-19 infection and the Coroner found that “nothing could be done”, or “no other steps could have been taken” to have materially altered the eventual outcome for these residents.
The inherent assumptions of the Coroner’s findings were that COVID-19 was fatal for all the residents; that COVID-19 was untreatable; and that chemical restraints did not cause the deaths.
There is strong evidence to refute all of these assumptions, and it was not considered at the inquest.
The inquest also revealed how one COVID-19-negative resident, Barry Jehan, was unlawfully prohibited from leaving Newmarch House to be with his family because the risk he could pose, if he might have had the virus, to his family. Barry would later contract COVID-19 at the facility, be prescribed Midazolam and Morphine, and would succumb to a death “from COVID-19” five days after his COVID-19 diagnosis.
As we speculated in Part 1, although COVID-19 might have been a contributing factor in these residents’ “COVID-19 deaths”, it was the use of chemical restraints — namely Midazolam and Morphine — which hastened their deaths. It was also the denial of other potentially life-saving treatments or care that might have averted the allegedly fatal progression of these residents’ COVID-19 disease.
We now have several reasons confirming our hypothesis:
The sudden onset of the COVID-19 outbreak at Newmarch;
The curious appearance of Midazolam and Morphine at Newmarch House; and,
The rapid “time-to-death” for many residents following their COVID-19 diagnosis (and placement on the “end-of-life” treatment protocol).
The sudden onset of the COVID-19 outbreak at Newmarch
The COVID-19 outbreak at Newmarch House was the result of indiscriminate PCR testing of residents commencing on 14 April 2020.
The catalyst for the whole-of-facility testing was a positive test result for a Newmarch staff member, first reported on 11 April 2020 following a PCR test from 10 April 2020. At the same time, a resident at Newmarch (referred to as “CA” in the Coroner’s findings) undertook a PCR test because they were experiencing symptoms of COVID-19, including breathing difficulties.
“CA” was the only Newmarch resident to have demonstrated COVID-19-associated symptoms prior to the outbreak and discovery of these “COVID-19 cases”.
These other “COVID-19 cases” were not discovered because the residents were displaying symptoms that prompted testing. There are, therefore, several possible interpretations of this outbreak at Newmarch commencing on 14 April 2020:
These “COVID-19 cases” were false-positives resulting from the use of a flawed diagnostic tool for the detection of COVID-19;
These “COVID-19 cases” resulted from “aggressive swabbing” as described at the inquest by Dr. James Branley, the lead clinician managing the outbreak at Newmarch, which might have collected more cellular debris from dead (non infectious) SARS-CoV-2 cells:
“So my recollection is there was very much a debate at that stage, you just sit tight and you wait till people get symptomatic, and you swab them if they're symptomatic. Now that wasn't the approach that I took, I took the approach to systematically go in and swab aggressively.”1 [emphasis added]
These 15 newly discovered “COVID-19 cases” had contracted the SARS-CoV-2 virus days or weeks previously and were clearing the virus without it causing COVID-19 disease; and,
Some or many of these new “COVID-19 cases” were incubating the SARS-CoV-2 virus, whilst the infection was still in its early stages and progressing to a more advanced stage of COVID-19 disease.
The discovery of 15 additional “COVID-19 cases” could have resulted from a combination any or all of the above.
With the exception of “CA”, the residents had not demonstrated any of the laundry-list of COVID-19-associated symptoms to have warranted testing, and therefore, it is as though the 15 new cases were almost discovered accidentally in symptom-free residents who might have been unaffected by COVID-19 disease. Though Newmarch House was in lockdown from 23 March 2020, it was not placed into “full lockdown” (isolating residents in their rooms) until 12 April 2020 and so, it was not as though any COVID-19-associated symptoms could have easily been missed or ignored by the nursing staff or doctors at Newmarch House once the residents were isolated and neglected in their rooms.
If these new “COVID-19 cases” were at the earliest stage of infection, then the rapid disease-progression raises serious questions about the true causes of the “COVID-19 deaths” at Newmarch House, and the likely causative role played by sedation.
Sadly, it was the detection of these “COVID-19 cases” that initiated the prescribing of “anticipatory” or “crisis” medication to “manage” the outbreak.
The curious appearance of Midazolam and Morphine at Newmarch House
On 18 April 2020, Midazolam and Morphine “just all arrived” at Newmarch House, with registered nurse Christine Giles expressing uncertainty about who had placed the order in her evidence given at the inquest:
“I was told that they'd been ordered by the VACS (Virtual Aged-Care Service) team. They weren’t that they were ordered by the VACS team. They just all arrived, because I haven’t really, I didn’t really get told that they were all arriving. They arrived at 8 o’clock or something that night 9 o’clock that night, and then I had to try and block them all up. . . I guess we don’t normally order crisis medication or that medication until we've got somebody who’s dying. So, the fact that I had all of this medication arrived, I thought at the time I thought I thought oh my god, there’s an expectation that every one of these residents is going to need this medication, and . . . that hit me for a sixer, to be honest, at the time. I yeah. But I'd also heard it on the media about people dying left, right, and centre overseas. So, I guess it just hit me hard at that time.”2
In fact, so much of these restricted, “Schedule 8” drugs were sent to Newmarch House, as described in Nurse Giles’s evidence above, it “creat[ed] an acute problem of finding adequate locked storage space in which to store them.”3
VACS nurse practitioner Hailey Carpen, in her evidence at the inquest, suggested the prescribing of “anticipatory” or “crisis” medications — chemical restraints — for these residents was only as a “just-in-case” measure:
“So, anticipatory medications have been used by registered nurses for a long time, where they use their assessment skills to determine if a resident needs a particular medication, and so it would have been no different in this case. With COVID, the use of anticipatory medications in these patients would be just as clinically indicated as other patients who didn't have COVID who were possibly at, you know, approaching end of life or in distress. . . I think mostly they were prescribed because of the uncertainty of the way each patient, or each person would react to becoming COVID positive, and so if they needed the medications, they were there.”4 [emphases added]
Carpen’s evidence is confusing. She stated that chemical restraints were prescribed because of the uncertainty of the way each patient would react. But, prescriptions would typically only be issued for a medical need, not as a precaution for uncertainty.
If these medications were pre-prescribed for all COVID-positive residents, that suggests they were being set up for “end-of-life” use regardless of symptoms.
The nurses and doctors working with VACS made every attempt to deflect from the inappropriateness of these chemical restraints. Doctor Mohammed Kakkat, the senior hospitalist in geriatric medicine for VACS, in his evidence before the inquest, described a situation where a number of residents were “declining rapidly” yet individual assessments of each patient were made:
“Remember, all the patients need to, need to assess individually, not a blanket thing, right. And if the patient had so many co morbidities [sic] and COVID came in between, so there is more chance to get it worse, right. . . We need to assess the patient, and as I told you before, we need to assess the patient, and prescription is individually based, not a blanket based. It is individually. If indicated, we have to prescribe.”5
When asked why the medication was prescribed in anticipation of symptoms being present, as opposed to being responsive to present symptoms, Dr. Kakkat explained:
“If the symptoms occur, that is the PRN [pro re nata or “as needed”], right. Now, we know that these symptoms can occur in this patient, right, so the trajectory is going like that so if these symptoms occur we don't need to run around that time, so we have a plan. That is the plan. This is a plan. This is not a must you must give the anticipatory medicines or crisis medication; this is a plan so if this happens, do this.”6
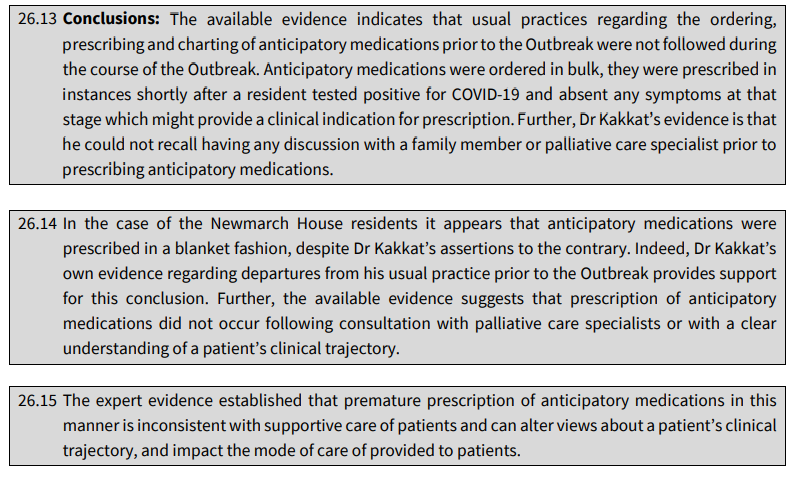
Yet the Coroner found Dr. Kakkat’s evidence particularly untrustworthy, concluding:
In sum, Midazolam and Morphine suddenly “arrived” at Newmarch House; was ordered in bulk; the medicines were used in a blanket fashion “shortly after a resident tested positive for COVID-19 . . . absent any symptoms”; and neither family members nor palliative care specialists were consulted or notified about the treatment.
Does it not all sound very suspicious?
Who gave the order to send the Midazolam and Morphine to Newmarch House?
Why did the VACS team rush to prescribe and administer these sedatives prematurely?
Incredibly, despite this alarming evidence, the Coroner would conclude that these resident deaths were all “COVID-19 deaths” — the eventual outcome which could not have been averted — only delayed.
The Coroner and the “experts” at the inquest should have more deeply interrogated the manner of death of those residents, particularly those who succumbed to a “COVID-19 death” so soon after their initial COVID-19 diagnosis.
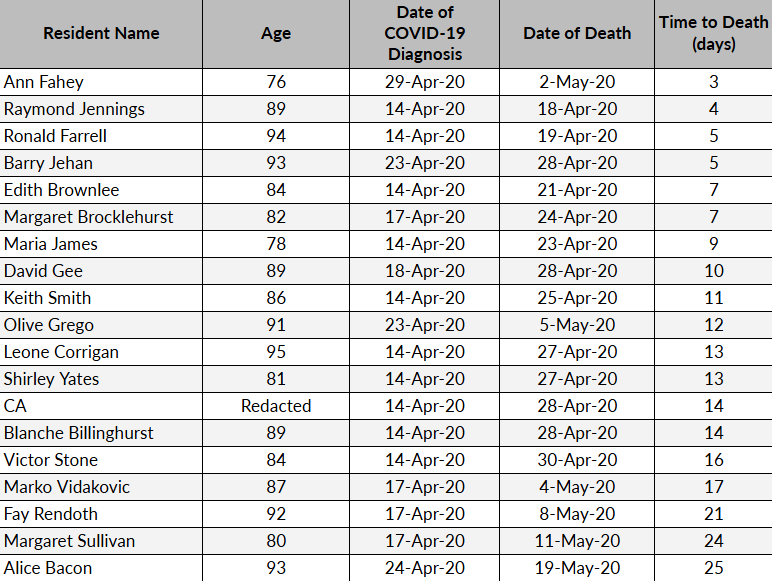
The rapid “COVID-19 deaths” of many Newmarch House residents
The rapid escalation of disease-progression in a number of “COVID-19 cases” leading to their “COVID-19 death” — only days later in some cases — raises serious questions about the true cause of these “COVID-19 deaths” and the standard of care provided for COVID-19 positive residents.
In 2020, “COVID-19 deaths” in Australia (the majority of which were in RACFs) had a mean time between diagnosis and death of 18.1 days which showed no evidence of varying by age.7 Yet, at Newmarch House in 2020, there were six resident “COVID-19 deaths” where the time from diagnosis to death occurred within a week or less:
Ann Fahey
Ann Fahey was the last of the group of residents to test positive to COVID-19, who died only three days after her COVID-19 diagnosis.
Her Advanced Care Plan (ACP) clearly stated that she wanted to be transferred from Newmarch House to hospital, if medically indicated (importantly, one of the indications for her to be transferred to hospital was for a fall) and wanted CPR and to be kept alive by being fed artificially. In sum, Mrs. Fahey did not have a “do not resuscitate” plan in place at any point.
On several separate occasions, Mrs. Fahey’s family were asked to confirm, however, if the “do not resuscitate” plans were still in place for Mrs. Fahey, first by Dr. Kakkat of the VACS team, and again when she was finally admitted to Nepean Hospital before her death.8
Mrs. Fahey’s family had wanted her to be transferred to hospital, but Dr. Kakkat, among others, wanted her to remain at Newmarch, in breach of her ACP. Mrs. Fahey had suffered a “minor fall” on 30 April 2020 which she described to her son as “losing her balance”, and no injury or pain was reported by her treating nurses. As per her ACP, however, a fall should have resulted in her transfer to the hospital, but it did not occur.
By 1:30am on 2 May 2020, Mrs. Fahey was evidently recovering well from her newly diagnosed bout of COVID-19, her attending nurse reported that she had “nil cough, respiratory distress pain or discomfort”.9
Yet, on 6:30am the same day, Mrs. Fahey was transferred to Nepean Hospital where, on admission, her condition had allegedly suddenly deteriorated to the point where the medical specialist noted:
“Impression: respiratory distress due to covid [sic]”.10
Which signed Mrs. Fahey’s death warrant.
By 10:36am on 2 May 2020, she was administered ketamine and fentanyl and was intubated.
She was extubated at 4:00pm on 3 May 2020 and died at 4:06pm.
In the five hours between 1:30am and 6:30am on 2 May 2020, Ann Fahey had progressed from “nil cough, respiratory distress pain or discomfort” to the near total opposite — “respiratory distress due to COVID-19” requiring intubation — then “COVID-19 death”.
She was the only resident at Newmarch House to have died “from COVID-19” not to have been prescribed Midazolam and Morphine, which the Coroner found was an oversight rather than a deliberate decision.
Mrs. Fahey’s transfer to Nepean Hospital was likely the result of her son Mark appearing in a Channel 7 evening news segment on 1 May 2020, criticising the standard of care at Newmarch House.
Had Mrs. Fahey not been transferred to Nepean Hospital, the evidence suggests that she most likely would have been prescribed Midazolam and Morphine and the eventual outcome would have been a “COVID-19 death” at Newmarch House instead.
Raymond Jennings
Raymond Jennings was first diagnosed with COVID-19 after the commencement of the whole-of-facility testing on 14 April 2020.
On 15 April 2020, Mr. Jennings did not complain of any pain and he sounded well, despite lower oxygen saturation and a slightly elevated temperature. These symptoms continued to 16 April 2020, where he was reported as “awake, alert and coughing, but not in pain or distress”.11
At this point the VACS team and Dr. Kakkat became involved, as the Coroner wrote:
“At 4.05pm, Mr Jennings was reviewed by the VACS team, including Dr Kakkat. The note was limited to a record that Mr Jennings was ‘93 yrs old male 125 not for transfer with hospital with COVID +ve’, a list of his comorbidities, and observations identical to those recorded at midday by a care worker. Anticipatory medications were charted by Dr Kakkat, including morphine, but there is no record that these were clinically indicated, discussed with family, or in fact administered.”12 [emphasis added]
The Counsel Assisting submitted that Dr. Kakkat likely copied the notes from an earlier observation, without even conducting a face-to-face assessment of Mr. Jennings; or perhaps not at all.13
By 17 April 2020, Mr. Jennings’s lower oxygen saturation and fever persisted, but he was not experiencing any breathing difficulties. Yet, Dr. Branley opined “he did not think [Jennings] would recover” in a phone-call with Jennings’s daughter that same day.14
By 18 April 2020, Mr. Jennings’s oxygen saturation and fever had improved, his blood pressure and respiratory rate were all within the normal range. He was communicative and denied pain. By 9:56am he was assisted with breakfast and had his usual medications.15
At approximately 10:30am, half-an-hour later, he was found not breathing, with no vitals, no pulse, cold skin and his face turned blue and he was confirmed deceased.
The Coroner found that Raymond Jennings died “from COVID-19” and his death was quite sudden and no other outcome was likely in the circumstances.16
Though the Coroner found no evidence that Midazolam and Morphine were administered, the detailed evidence presented in the Coroner’s findings from the observations of Mr. Jennings suggest that he was, in fact, sedated:
In severe hypoxia (oxygen saturation rates below 85%), the body usually compensates by breathing faster, yet Mr. Jennings’s respiratory rate dropped to 14 breaths per minute in his final hours instead of increasing;17
Despite persistently low oxygen saturation, there were no reports of gasping, struggling, or visible distress, suggesting a blunted physiological response, likely from sedation;
Earlier, on 17 April, his body showed signs of compensation with high blood pressure, an elevated heart rate, and fever. However, by 18 April, instead of worsening, his blood pressure stabilised, his heart rate slowed, and he remained communicative until shortly before he was found unresponsive, suggestive of sedation;18 and,
In acute respiratory distress, patients typically struggle for breath before collapse, yet Mr. Jennings did not show this pattern. Instead, his body stopped compensating, suggesting that his respiratory drive had been suppressed, likely because of sedation.
Raymond Jennings had a “do not resuscitate” plan in place.
His was Newmarch House’s first “COVID-19 death”.
Ronald Farrell
Ronald Farrell had a case of “COVID-19” that was reported by the staff at Newmarch to be “mild” as late as 18 April 2020 — just days before his “COVID-19 death”.
Despite vitals within the “normal” range, albeit with oxygen support, Dr. Kakkat prescribed Midazolam and Morphine for Mr. Farrell on 17 April 2020 with the Coroner taking a very dim view of the decision:
“Dr Kakkat was questioned in relation to his clinical thinking for prescribing anticipatory medications for Ronald Farrell in circumstances where the Nepean clinical record entry records no vital signs. He gave evidence that if he wrote anticipatory medication there would be a [clinical] ‘indication’ and that “it is not a blanket thing.” Dr Kakkat was unable to give any clinical justification for prescribing anticipatory medications. He said that the medications were prescribed as anticipatory of any symptoms, namely pain, shortness of breath, agitation, irritability, for vomiting, for nausea, and ‘these types of symptoms.’ Of note is that Ronald Farrell had none of these symptoms at the time of the prescribing of the anticipatory medication.”19 [emphasis added]
Morphine was commenced for Mr. Farrell only an hour before he died “from COVID-19” at 6:00am on 19 April 2020, as recorded in the findings.20
But, as was the case with Raymond Jennings, strong evidence suggests that the prescribing and administration of “anticipatory medication(s)” occurred as early as 17 April 2020 — coinciding with Dr. Kakkat’s prescribing. These reasons include:
On 17 April, when Mr. Farrell’s oxygen saturation dropped to 84% (severe hypoxia) without supplemental oxygen, his respiratory rate was only 22 breaths per minute, which is mildly elevated but not extreme. Normally, with severe hypoxia, a much higher rate would be expected as the body struggles for oxygen;
On 18 April, when Mr. Farrell’s oxygen dropped to 84% (severe hypoxia) again, his respiratory rate remained at 22 breaths per minute, showing no significant increase despite worsening oxygen levels;
Overnight on 19 April, despite continued severe hypoxia and a raised respiratory rate, by 4:15am that same day, Mr. Farrell was observed “sleeping comfortably”.21 If Mr. Farrell was in severe respiratory distress, it would be highly unusual for him to be sleeping peacefully, suggesting he was sedated.
Though the experts at the inquest agreed that escalating care could have been provided to Mr. Farrell, perhaps with antibiotics or better oxygen administration and management, there was a consensus among them that nothing could have been done that would have materially altered the eventual outcome for Mr. Farrell.
Despite the assurances from the Newmarch House staff that his case was only “mild” when diagnosed on 14 April 2020, his death only five days later, became Newmarch House’s second “COVID-19 death”.
Barry Jehan
Barry Jehan was another “sudden death” at Newmarch House “from COVID-19”.
Twice, Mr. Jehan had tested negative to COVID-19, yet, he was still prohibited from leaving the facility by Newmarch House for the risk he could pose to his family if a mysterious infection had not been detected by the PCR tests at Newmarch.
Progress notes, taken just ten minutes after Mr. Jehan died (at approximately 3:10am) stated:
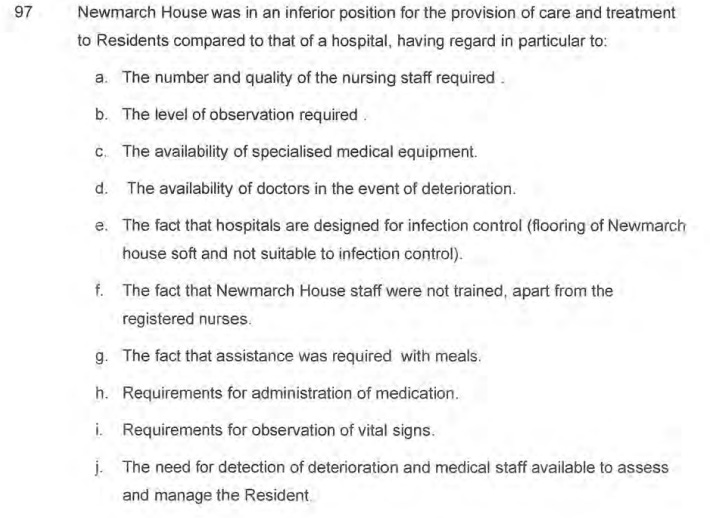
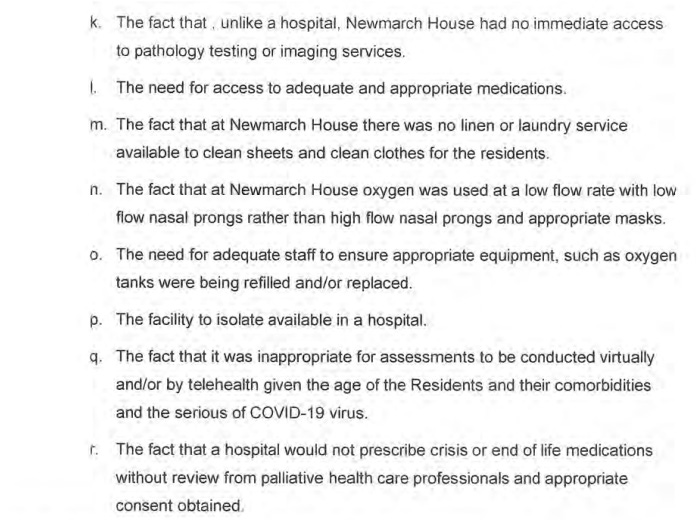
“Mr Jehan has died just now. I last saw him at 2.40am and he was quite comfortable then, I had prayed with him at around 2.30am and deterioration noted in respiratory effort but he was quite comfortable.”22
The suddenness of the “COVID-19 death” is peculiar as well for the evidence at the inquest about Mr. Jehan’s apparent recovery by the evening before he died:
“At 9.00pm [on 27 April 2020], a RN [registered nurse] spoke to Ms Van Put, and told her than Mr Jehan was comfortable and well looked after. Mr Jehan was noted to be asleep, but rosary attended to with classical music playing. Ms Van Put gave evidence that a nurse called Ursula told her that her father was eating three meals a day, that he was chatting on about being a signalman and his classical music and that she had “good feelings” about him (alluding to his recovery).”23
Mr. Jehan was comfortable and well-looked after and there was a sense of his impending recovery, yet, he was dead six hours later “from COVID-19”.
There is, once again, strong evidence suggesting that he was prescribed and administered Midazolam and Morphine, causing his “COVID-19 death”:
Dr. Kakkat prescribed both medicines well-before any escalation of Mr. Jehan’s COVID-19 symptoms on 25 April 2020 — in keeping with Dr. Kakkat’s improper “just-in-case” approach of prescribing “end-of-life” medicines without the clinical indication to do so (as noted by the Coroner in his conclusions24);
Though the Coroner found that the “medication charts [did] not disclose any administration of either Morphine or Midazolam”25, the consistent and serious problems with Newmarch House’s management and processes reveal that the lack of disclosures of the use of these sedatives might not mean they were not being used; rather, that they were not being documented:
“Mr Jehan was noted to be very breathless, and an RN phoned a doctor for a telephone order of oral Morphine which was noted to be ‘effective’ although there is no record of morphine being administered.”26
Were staff simply too busy to maintain these essential patient records, or did someone deliberately try to conceal the use of these medicines by not keeping complete patient records?
Edith Brownlee
Edith Brownlee tested positive to COVID-19 on 14 April 2020, when the whole-of-facility testing was commenced.
Just three days after her COVID-19 diagnosis, on 17 April 2020, VACS nurse Hailey Carpen prescribed Midazolam and Morphine.
The Coroner’s findings did not address whether these sedatives were administered, however, it is clear that Mrs. Brownlee’s case of COVID-19 was mild and the medicines were inappropriate, and, as with the other cases discussed so far, not clinically indicated for Mrs. Brownlee.
Even more concerningly, the sedatives were ordered despite no observations having been recorded:
“At 5.26pm RN Carpen from VACS recorded that observations were not recorded and yet “anticipatory end of life medications ordered today.” Whether there was a remote review of the notes, or an inperson review, is unclear. RN Carpen also completed the medication chart.”27 [emphasis added]
Mrs. Brownlee had a “do not resuscitate” plan in place and as the Coroner described, she was essentially left alone to die at Newmarch House:
“There is no record to indicate that Edith Brownlee was seen by any Hospital in the Home (HITH) or VACS team member (medical or nursing) between 17 April 2020, and the time of her death on 21 April 2020. The only entries between those dates involved a remote review of the Newmarch House progress notes. There is likewise no evidence in the Newmarch House clinical records that Mrs Brownlee was seen by a GP after 8 April 2020.”28
The evidence presented at the inquest showed that Mrs. Brownlee’s vitals all remained within the regular range, she was “alert and interactive”, and less than 12 hours before she died “from COVID-19”, she was described by one nurse to be:
“[D]oing really good and her oxygen and mood was good”.29
The Coroner did not address whether the Midazolam or Morphine was actually administered to Mrs. Brownlee, but again, the detailed observational evidence from the nursing staff at Newmarch suggest that she was sedated:
Mrs. Brownlee’s vital signs were not as extreme as the other cases, but the drop in her oxygen saturation and lack of distress suggest the effects of sedation. Her respiratory rate spiked at 9:34pm on 20 April 2020, which indicated her body initially attempted to compensate for something, but it then returned to normal by 10:00pm despite her oxygen saturation decreasing, suggesting her respiratory drive was subdued, likely from sedation; and,
On 21 April 2020, registered nurse Tegan Dean noted:
“[A]febrile [observations] stable asymptomatic meds given as ordered”.30 [emphasis added]
Recalling that “crisis medications” — Midazolam and Morphine — were ordered on 17 April 2020 for Mrs. Brownlee by Nurse Carpen, it is plausible that the “meds given as ordered” were these sedatives which hastened Mrs. Brownlee’s death “from COVID-19”.
Summary
The Coroner’s findings in the “Inquest into the Deaths at Newmarch House” reveal a horrifying picture of what constituted residential “aged-care” in 2020.
It is deeply troubling to reflect on the COVID-19 panic which paralysed our public health response. Residents at Newmarch House were essentially detained and their loved ones believed the propaganda of an ambitious program named “Hospital in the Home” (HITH) and what it could offer.
But, HITH was never capable of delivering its two central aims — to improve a patient’s experience during episodes of acute illness and reduce disruption to family life — when faced with the myriad challenges tossed-up by the ever-changing public health landscape.
Under this model, residents did not receive daily care and clinical review until 28 April 2020, by which time 12 residents had already died “from COVID-19”.31 The “aged-care” offered under this model was characterised by isolation and neglect.
The VACS model was revealed to be equally horrific. The Coroner highlighted that geriatric medical assessments should be conducted face-to-face, rather than via telehealth or screens, making the VACS model particularly inappropriate for RACF settings. On the limited occasions where the VACS team attended Newmarch, such as in the first two weeks of the COVID-19 outbreak at Newmarch, the VACS team “did not always see patients” and on the limited occasions where face-to-face consultations occurred, there was no follow-up after the initial consultation and the progress notes were not always recorded in relation to these consultations.32
The seemingly “hands-off” and “screens-on” approach of the VACS team was described by Nurse Carpen in her evidence at the inquest:
“So, the VACS team was sitting at the hospital in front of a computer. The team in the nursing home would take a device into a resident. We would talk to the resident Dr Sharma would talk to the resident and find out about their symptoms, obtain the observations from the nursing staff at the time, and come up with a plan.”33
The Coroner was critical in his summary of the approach and usefulness of the VACS standard of “care”:
“The telehealth reviews were largely focused on discussions around not transferring patients to hospital. Other than recording the prescription of anticipatory medications, the available records do not indicate that any thorough medical assessment was performed, or any treatment or management plan formulated. For example, the available records do not indicate that any comprehensive geriatric assessment was conducted for any resident.”34 [emphasis added]
Evidently, the VACS team were more preoccupied with keeping the residents at Newmarch House rather than transferring them to hospital where they could have a higher quality of care and treatment.
The VACS team were equally preoccupied with prescribing sedatives for COVID-19 positive residents, ordering them in bulk in anticipation of illness, despite having no clinical indication for doing so.
Rather than simply providing palliative comfort or allowing a natural end, the protocol appears to have hastened death in a manner some might characterise as “active involuntary euthanasia”; when a medical intervention takes place, not at the patient’s request, in order to end the patient’s life. As the expert evidence at the inquest established, the premature prescribing of “end-of-life” medicines was “inconsistent with supportive care of patients”.35
If it wasn’t supportive care, and if the intent to hasten death existed, some legal interpretations could consider it euthanasia. Alternatively, if sedatives were administered in a reckless or negligent manner, there could be grounds for a claim of unlawful practice.
In April 2023, a class action was initiated against Anglicare Sydney and the Nepean Blue Mountains Local Health District concerning the outbreak at Newmarch House, testing these very claims. The lawsuit, led by Shine Lawyers on behalf of 18 affected family members, alleged negligence in managing the outbreak and resident care.
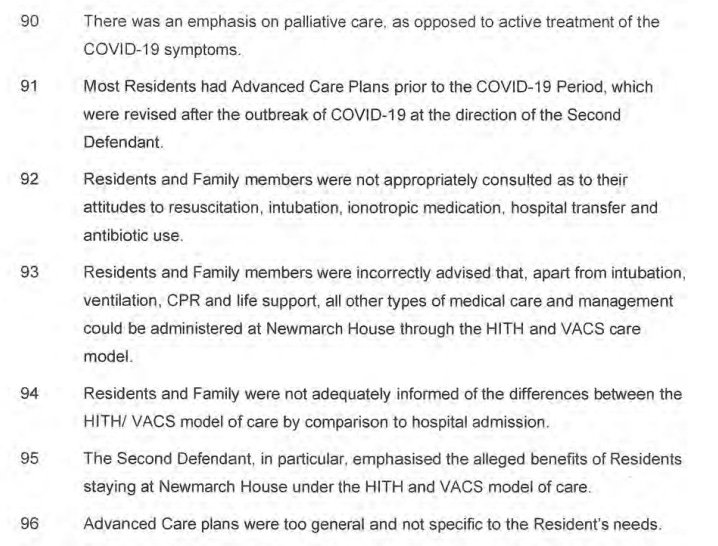
The allegations in The Statement of Claim lay bare the appalling standard of care at Newmarch, including the prescribing and administration of Midazolam and Morphine, the isolation and neglect of the residents, and the abject failures of Newmarch House’s management of its COVID-19 outbreak commencing in April 2020 (see below):
In November 2024, a confidential settlement was reached and is now pending court approval, to be decided on 2 May 2025.
Despite the wishes of the families of the Newmarch House residents, would anyone have been better off in hospital in 2020?
Sadly, probably not.
We have every reason to believe that a similar “end-of-life” protocol would have been applied to COVID-19 positive residents had they been transferred from Newmarch House.
Remember, the only box we had to tick to place one on an “end-of-life” protocol was the “recovery is not expected” box before recommended sedatives could lawfully be used in the treatment of a COVID-19 positive patient.
Ann Fahey’s sad story is a stark reminder of how quickly an aged, comorbid, COVID-19 positive resident could deteriorate and die a “COVID-19 death” once admitted to hospital in 2020.
The assumptions made by the Coroner in his findings — COVID-19 was fatal for all the residents; that COVID-19 was untreatable; and that chemical restraints did not cause the deaths — were all influenced by the medical professional “experts” in their evidence at the inquest.
And although the coronial inquest took many years to conclude (meaning the “expert” evidence was given years ago), it would be uncontroversial to assume that these assumptions about COVID-19 would persist for many “experts” today too.
Though the legacy media covered the findings of this inquest, most of the commentary predictably focused on simple variations of the same theme:
“We didn’t get them to hospital quickly enough”.
“It was the lack of leadership with poor communication”.
“We didn’t test hard enough, we could have caught more cases earlier!”
As though the crisis at Newmarch House could have been solved by finding more “COVID-19 cases”.
The crisis at Newmarch House was the subject of several separate reviews, and just like the legacy media reports, all of them decided to focus on every issue aside from those which were most important.
Nothing about chemical restraints.
Nothing about how all the residents who died in the outbreak at Newmarch House were prescribed Midazolam and Morphine in advance of their illness.
Nothing about how Midazolam and Morphine were ordered in bulk and sort of “just all arrived” at Newmarch House after the outbreak in a bulk quantity so large it created an acute problem of where to store the medicines.
It was preferable to pretend it was chaotic and directionless at Newmarch House rather than to interrogate why “end-of-life” protocols were adopted for COVID-19 positive residents, or the ways that Midazolam and Morphine caused the “COVID-19 deaths”.
These predictable omissions and diversions are a sad indictment on the integrity of those responsible for inquiring into the “COVID-19 deaths” at Newmarch House in 2020.
The dangers of these sedatives were well-known before the pandemic, even when administered to relatively healthy people:
“Midazolam, a short-acting drug also used to combat seizures, has well-known side effects including the slowing – or even stopping – of breath . . . . Dr Minh Le Cong of the Royal Flying Doctors Service, said in his experience administering Midazolam to patients would often be either “ineffective, or too effective. You’d either just keep giving more and more doses, or then when it did work it would work too well in that the person would be in a medically induced coma” he said. . . . Dr David Taylor, who has studied the use of Midazolam in Victorian emergency departments, said hospitals have strict procedures and guidelines in place. “It’s always mandated that you have someone giving the drugs to sedate the patient, and another person who is there observing the patient” said Taylor. “Managing the risks of Midazolam outside the controlled environment of the emergency room is more difficult and if staff don’t have the training and equipment to pick up the side effects or manage them appropriately then it could be a potentially dangerous situation”.36 [emphasis added]
Yet, the COVID-19 pandemic has taught many how to be wilfully ignorant and how to suspend rational inquiry if the slightest chance a “COVID-19 conspiracy” is detected.
It is disheartening, but we are on the right side of history and we must keep challenging the pandemic narrative.
Even if these stories are never explained or acknowledged publicly, and the perpetrators do not face consequences, these truths will be learned by more and more people and that alone is worth every continued effort.
In the next article, as promised, we will reveal our analysis of the prescriptions and medicines shortages data from beyond 2020.
As we wrote in our last article:
“Something made Australia sicker in 2021 and palliative care prescribing soared from mid-2021 onwards.”
Thank you for reading.
Coroner’s Court of New South Wales, Inquest into the Deaths at Newmarch House, findings by Magistrate Derek Lee, Deputy State Coroner, January 24, 2025, [16.6-16.7]
Ibid., [26.1-26.2]
Gilbert, L. and Lilly, A., “Newmarch House COVID-19 Outbreak [April-June 2020] Independent Review Final Report”, https://www.health.gov.au/sites/default/files/documents/2020/08/coronavirus-covid-19-newmarch-house-covid-19-outbreak-independent-review-newmarch-house-covid-19-outbreak-independent-review-final-report.pdf, p. 22.
Ibid., [26.3-26.4]
Ibid., [13.11 and 26.6]
Ibid., [26.7]
Marschner, I.C., “Estimating Age-Specific COVID-19 Fatality Risk and Time to Death by Comparing Population Diagnosis and Death Patterns: Australian Data”, BMC Medical Research Methodology, 21, 126 (2021). https://doi.org/10.1186/s12874-021-01314-w
Coroner’s Court of New South Wales, op. cit., [43.21]
Ibid., [43.44]
Ibid., [43.48]
Ibid., [30.18]
Ibid., [30.21]
Ibid., [30.22]
Ibid., [30.24]
Ibid., [30.27]
Ibid., [30.31]
Ibid., [30.27]
Ibid.
Ibid., [31.22]
Ibid., [31.30]
Ibid., [31.25-31.31]
Ibid., [37.38]
Ibid., [37.37]
Ibid., [26.13-26.14]
Ibid., [37.8]
Ibid., [37.36]
Ibid., [32.19]
Ibid., [32.6]
Ibid., [32.33]
Ibid., [32.34]
Ibid., [18.12]
Ibid., [24.19]
Ibid., [24.8]
Ibid., [24.9]
Ibid., [26.15]
The Guardian, “Doctors Issue Warning Over Tranquilliser Linked to Deaths in Custody”, https://www.theguardian.com/australia-news/2018/mar/06/doctors-issue-warning-over-tranquilliser-linked-to-deaths-in-custody, accessed 19 March 2025.





It's time to subpoena the banking and tax records of every hospital and all medical personnel involved in patient care in 2020-2022
Page 135 of the Inquest Report, para. 32.5.
60 mg midazolam administered. A fatal dose is 50 mg.
What a whitewash.